From Tumors to Spinal Damage—What a Neuroradiologist Does
by Nitasha Klar, MD, ARA neuroradiologist
Knowledge is power when it comes to protecting your health, especially in the case of a serious condition that might require a neuroradiologist. Let’s first talk about how one becomes a neuroradiologist. General radiologists go through four years of medical school, one year of internship and four years of general radiology residency and possibly an additional year of fellowship. Neuroradiologists do additional, specialized training of one to two years in length, becoming subspecialists in the imaging field that focuses on the head, neck and spine. I personally received my medical degree at Drexel College of Medicine in 2007. I did an internship and then a residency and fellowship at Johns Hopkins Hospital. I joined ARA just a few years ago and have really enjoyed practicing and living in downtown Austin.
Typically, neuroradiologists work very closely with other physicians, like general practitioners or specialists such as neurosurgeons or neurologists, who usually call the neuroradiologist in consultation. We put our heads together, look at the examination information, and decide on an imaging protocol that will bring an accurate diagnosis. Then the neuroradiologist uses his or her years of training and experience to determine what the images tell us about what is going on with the patient.
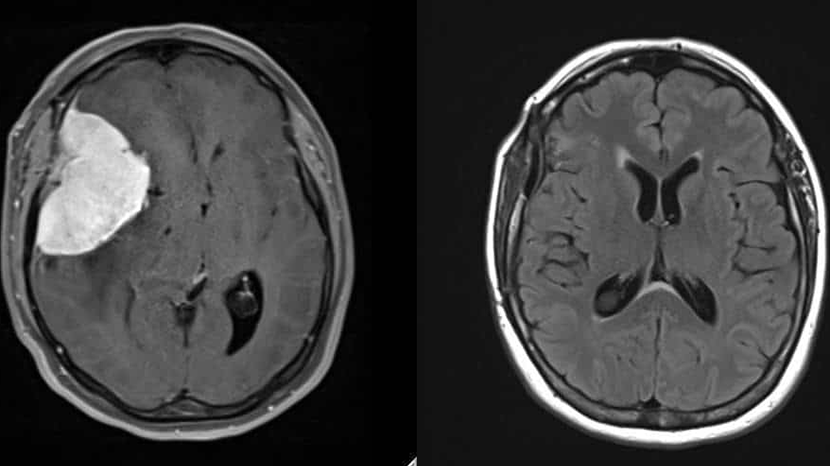
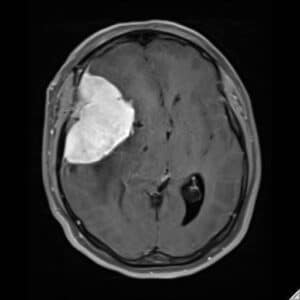
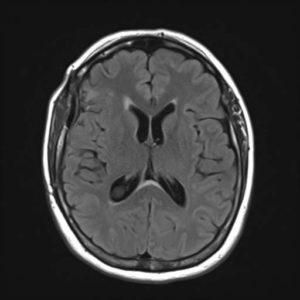
Our first image is an MRI of a patient who presented with headaches. The image shows a large mass that is actually pushing the brain out of shape within the skull. The very bright area on the image turned out to be a benign mass called a meningioma. The post-surgical MRI shows the brain having returned to a normal shape after resection by a neurosurgeon. The patient completely recovered. The neuroradiologist diagnosed the condition, the imaging helped guide and plan the operation, and the neurosurgeon removed the tumor.
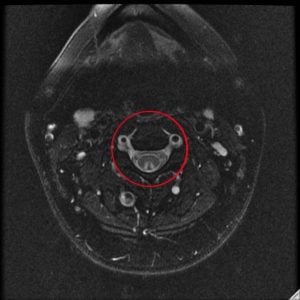
The second image is an interesting case of a young patient who came in with altered sensation in the extremities. We turned to an MRI to assess what was happening in the spinal cord that might be causing these sensations. What the MRI showed us —the triangular white presentation in the cross section image and the cloudy white appearance of the spinal cord in the side view—is specific to only a few conditions. In fact, this was a case of drug abuse. The patient had been inhaling nitrous oxide through whipped cream canisters and got spinal cord toxicity. That information had been withheld from the ER physician, and imaging was the vital point of examination that diagnosed the issue.
A variety of symptoms can lead a patient to need the services of a neuroradiologist. We encounter conditions as common as tension headaches and back pain, as well as stroke, tumors and trauma. According the American Society of Neuroradiology, “Neuroradiology is the clinical subspecialty concerned with the diagnostic radiology of diseases of the central nervous system, brain, head and neck, through the use of X-ray, MRI, CT and angiography. It is practiced in hospital settings, academic/educational institutions, and private practice.” While ARA hopes you never need a neuroradiologist, we are here to serve you with expertise and compassion.

 Back to Top
Back to Top