A myelogram is an imaging procedure that produces real time X-ray images of the spine using a technique called fluoroscopy. Myelograms can be performed on one of three sections of the spine—cervical, thoracic, or lumbar—or on all three at once. By injecting contrast material into the spine, doctors can visualize the spinal cord, nerves, and tissues that line the nerves (meninges). Myelography is typically used to evaluate the spine before and after surgery and to detect problems in patients who cannot undergo MRI.
Fluoroscopy is a medical imaging test that uses ionizing radiation (X-rays) to obtain images of structures inside the body. The images can then be viewed on a monitor in real time. Many structures, such as bone or a part of the body filled with contrast, can be examined with fluoroscopy.
In most cases, MRI is the exam of choice when evaluating spine abnormalities. Due to the strong magnetic field, some patients – like those with implanted medical devices – cannot undergo MRI. In these cases, myelography is a safe alternative. In other cases, myelogram is used when MRI does not provide enough detail about a spinal abnormality.
Conditions that can be evaluated by myelogram include:
- Herniated intervertebral discs causing nerve or spinal cord compression
- Spinal stenosis which is a narrowing of the canal where your spinal cord is located. Spinal stenosis is caused by degeneration of the bones and soft tissue in the spine.
- Tumors, infection, and inflammation around and in the spine
- Assessment of trauma to the spine
- When planning for surgery of the spine
Benefits
- Myelogram is a safe and highly effective way to evaluate problems with the spinal cord, nerve roots, and meninges.
- For patients that cannot undergo MRI, myelogram offers a safe alternative.
- The amount of radiation used in myelography is unlikely to increase your risk of cancer, and no radiation remains in your body after the exam.
- The risk of side effects due to the radiation used in myelography is minimal.
Risks
- Myelogram involves a needle puncture of the spinal canal. In very few cases, this can cause a headache within a few days after the procedure. Most spinal puncture headaches resolve with rest and medications. More persistent symptoms may require a procedure called an epidural blood patch.
- Fluoroscopy uses a low dose of radiation because it uses X-ray technology, but the benefit of an accurate diagnosis far outweighs the risk. Please refer to the Fluoroscopy page for more information on the risk of radiation used in this exam.
- Pregnant women should be aware of the risk of radiation to the developing baby. For more details, please refer to the Fluoroscopy page.
- Other rare complications of myelography include nerve damage, infection, seizures, and spinal fluid obstruction which requires urgent surgical care.
- Myelography is done at an ARA imaging center. The exam takes about 30-60 minutes and you will need to rest in recovery at the center for about 2 hours.
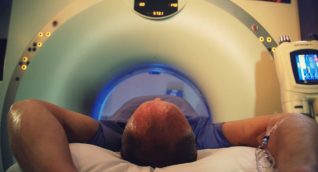
- You will be asked to change into a gown and placed on an exam table with a special X-ray camera nearby that uses fluoroscopy to take moving images of your spine. Initially you will be lying face down, or prone.
- The injection site near your spine will be cleaned using sterile technique, and the area will be numbed using an injection of a local anesthetic called lidocaine. Lidocaine does sting for a few seconds, but the area goes numb very quickly.
- Once, the area is numb, the radiologist will insert a spinal needle into your back under guidance of the fluoroscope until the needle reaches the arachnoid space. This is a fluid-filled space that surrounds and cushions the spinal cord.
- Once the needle is in place just inside the arachnoid space of the spine canal, fluid will move into the needle. The radiologist will then slowly inject the clear X-ray contrast fluid through the needle and into the spinal fluid sack. This may cause some pressure or even and increase in your current symptoms, temporarily.
- The contrast is not radioactive. It shows up on X-ray because the atoms of iodine within the contrast make the fluid visible. Once the radiologist injects the amount of contrast needed, he/ she will remove the needle. The soap will be wiped off your skin and a band-aid will be placed over the injection site.
- Depending on which area is to be studied, the contrast will be moved up or down the spine with gravity. If the lumbar spine is of interest, you will be slowly tilted on the table to a standing position. Images will be taken in different upright positions. If the cervical spine is the area of interest, the table will be tilted so that your head is slightly lower than your body. Shoulder supports will be used to keep you from sliding out of position. Your chin will be placed on a sponge to prevent the contrast from rolling into your head and causing a headache. Once the contrast is in the cervical spine, the table will be flattened, and images will be taken with your neck in different positions.
- If the thoracic spine is of interest, you will be asked to roll onto your side or back. The contrast will coat the thoracic area and images will be taken in different positions.
- After the initial myelogram exam, you will be taken by stretcher to the CT suite for imaging of the area/areas of interest. The CT part of the exam shows the very specific details of the nerve roots as well as the bony anatomy.
- Any discomfort is usually mild and temporary. You will be asked to avoid exertion for the rest of the day to prevent a headache. You will be released from the recovery bay after 2 hours after the injection.
- You will be asked not to eat for a several hours prior to the myelogram. You should drink plenty of fluids to remain well hydrated. In most cases, you should take all your medications as usual. However, if you take any blood thinners, aspirin, antipsychotic, or antidepressant drugs, ask your doctor about stopping these medications. You may have to discontinue them several days before the exam.
- Be sure to tell your radiologist about any illness or allergies you may have. Also, provide a list of your current medications.
- Inform your radiologist if you are pregnant. Although the risk of myelogram is very low for the unborn baby, your doctor may choose an alternate exam. Depending on the circumstances, both the physician and patient may decide it is necessary to go ahead with the exam. Pregnant women should not undergo X-ray or receive contrast unless the benefits clearly outweigh the risks.
- Some doctors recommend that breastfeeding women wait 24 to 48 hours until the contrast clears from their system before breastfeeding again. Before the procedure, breastfeeding women may want to pump breastmilk to have on hand for the time following the myelogram.
Your medical team may work with ARA’s radiologists to schedule the procedure at an ARA fluoroscopy suite or a local hospital. You can also schedule at (512) 453-6100.
A radiologist, a physician specifically trained to interpret radiological examinations, will analyze the images and send a signed report to the provider who referred you to ARA. The physician will then share the results with you.