ARA offers minimally-invasive, highly successful treatment for peripheral arterial disease (PAD) that will bring relief from swollen legs, distended veins, and circulation-related ulcers.
Peripheral artery disease treatment uses interventional radiology techniques to restore circulation, most commonly to the legs.
Peripheral arterial disease, or PAD, is a condition in which the arteries are not delivering enough blood to the legs because of plaque collection or other substances that narrow or block the artery. This means that the tissues of the legs are not getting enough oxygen. The earliest symptom is leg pain or cramping while walking that improves when resting. As symptoms progress, you may have more pain which can become severe. A person with a very advanced case of PAD may also have wounds that develop from a minor injury that won’t heal or such severe disease that amputation has to be considered.
Most people are aware that arteries can develop plaque and blockages that affect your heart and put you at risk of a heart attack. The arteries in your legs can suffer from the same disease. The same risk factors for coronary artery disease that affect your heart, namely smoking, diabetes, high blood pressure, obesity, and lack of exercise can also lead to blockages in the arteries in your legs.
Interventional radiologists are board-certified physicians who deliver minimally invasive treatments for peripheral arterial disease with less risk, less pain, and less recovery time than traditional surgery. Your condition will most likely be evaluated before the procedure using CT, ultrasound, or MRI.
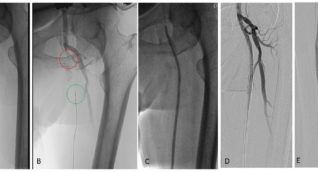
Angioplasty
Angioplasty uses inflatable devices called balloons to open up narrowed arteries. Various types of balloons are used in different situations, including balloons that stretch arteries open, metal-edged balloons that cut and break up calcium deposits, and drug-coated balloons that can prevent scarring and future narrowing of the artery.
Stenting
Stenting uses small metal mesh tubes to hold open narrowed arteries. Various types of stents are used, including two main categories:
- Bare metal stents:These are made of simple metal mesh, which allows the body to coat the stent with cells that prevent new blood clots from forming; however, this approach increases the chance that the artery may become narrowed by scar tissue.
- Drug-eluting stents: These are more modern and slowly administer medication to the blood vessel wall to prevent scar formation; but the medication also stops the body from coating the stent with protective cells that prevent new blood clots from forming. Patients who receive stents also need to be on clot-preventing medications related to aspirin called “anti-platelets” that reduce the chance of clots forming inside the stent.
Atherectomy
An atherectomy uses a tiny catheter inserted into a blood vessel to navigate to and remove hard arterial plaque. The catheter features a metal tip that shaves away arterial material and opens the vessel, allowing blood to flow. An atherectomy is especially useful in cases where blockages occur around arterial branches or in areas not easily fit with stents.
Thrombolysis
Thrombolysis delivers medication slowly, over 12-24 hours, to a blood clot through a thin tube that is inserted next to or within the clot. This treatment is usually done in an emergency because the body has not had enough time to respond by growing new blood vessels to bypass the blockage. The patient is hospitalized during the treatment and will be watched by nurses and doctors in the intensive care unit. Often, the clots will be dissolved but the artery will still be narrowed and additional treatments may be required.
Thrombectomy
When a blood clot suddenly blocks blood flow, a treatment known as a thrombectomy will remove the clot from the body using various medical tools that can draw out, pull out, or dissolve the clot. The method chosen depends on the preference of the physician and the location of the clot.
Peripheral arterial disease treatment also includes imaging techniques such as fluoroscopy, angiography, CT angiography, MRI angiography and ultrasound. Please refer to sections about these techniques for further details.
If you have peripheral arterial disease, you may have symptoms, such as:
- Leg pain, numbness, coldness or burning. This may only occur when you walk.
- Leg weakness
- Poor wound healing or sores on the feet or legs
- Skin and hair changes of the legs/feet
- Weak pulses in the legs/feet
If you have any of these symptoms, and a diagnosis of PAD is confirmed, your doctor may recommend treatment.
What are the benefits and risks of peripheral arterial disease treatment?
Benefits
- Peripheral arterial disease treatment is a much less invasive way to restore circulation compared to bypass surgery.
- By restoring blood circulation to the legs, PAD treatment may avoid serious complications such as poor wound healing, pain, or the need for amputation.
- Interventional PAD treatment only requires a small incision in the skin.
- PAD treatment can benefit your overall health, allowing you to exercise and be active without experiencing the pain and fatigue caused by blocked arteries.
- In the vast majority of cases, patients are released on the same day of the procedure.
Risks
- While extremely rare, there is a risk of allergic reaction to contrast material containing iodine. ARA radiologists are well prepared in the event of such a reaction. If you have had an allergic reaction to contrast material in the past, your radiologist may recommend that you take medication for 24 hours before the procedure to reduce risk.
- During the procedure a small puncture must be made in the skin for doctors to access an artery. Also, a catheter will be placed into the artery. Complications may include bruising, bleeding, hematoma, blood vessel damage and infection. In rare cases, surgical repair may be required. Your radiologists and technologists are trained to minimize the risk of complication.
- Pregnant women should avoid radiation exposure if possible. Talk to your doctor or technologist about the risks of radiation exposure if you are or might be pregnant.
- The American College of Radiology (ACR) says that current information suggests that breastfeeding is safe after the use of intravenous contrast. Please discuss your breastfeeding options with your physician.
- PAD treatment is typically done in an ARA imaging center, hospital or medical center. The procedure can take as long as 30 minutes up to several hours depending on its complexity.
- You may be asked to remove all metal and jewelry, and you will be asked to change into a gown.
- You will be placed on an exam table, and you will be connected to devices that monitor your blood pressure, heart rate and blood oxygen level.
- An intravenous (IV) line will be placed in a small vein of your hand or arm. You may be given a mild sedative. In some cases, general anesthesia is used.
- The skin over the blood vessel access site (usually the femoral artery in the groin) will be sterilized and covered with a sterile drape. You may be given an injection of local anesthetic. A small incision will be made at the site.
- A catheter will be inserted into the artery and guided to the part of your body that requires treatment.
- During the procedure, contrast will be injected into the artery to allow for visualization of the blood vessels and the area being treated. A special camera will take pictures which can be viewed in real time on a monitor by the interventional radiologist.
- Once the catheter reaches the area to be treated, special devices (described above) are used to either open a narrowed artery, break up a clot or remove blockage.
- More images may be taken to make sure the procedure was completed effectively.
- When the procedure is finished, the catheter is removed, and pressure applied to the incision site.
- You may be asked to rest in bed for 2 to 5 hours after the procedure after which most patients are allowed to go home. Depending on the complexity of the procedure, you may need to remain hospitalized for a few days.
- Wear comfortable, loose fitting clothing. You may want to leave all jewelry, piercings and any other metal objects at home.
- You will be asked not to eat or drink anything for up to 8 hours before the procedure. Ask your doctor for specific directions about your daily medications especially if you take any diabetes medication (insulin, etc.), blood thinners (aspirin, coumadin, warfarin, etc.) or NSAIDs (ibuprofen, naproxen, etc.).
- Be sure to tell your radiologist about any illness or allergies you may have. Also, provide a list of your current medications.
- Inform your radiologist if you are or might be pregnant. You doctor may recommend an alternate treatment if you are pregnant. Also, pregnant women should not receive IV contrast unless the benefits clearly outweigh the risks.
- Since you will be sedated, please plan to bring a friend or relative to drive you home. You will be kept for observation at the facility until you are cleared to leave and should not plan to drive for 24 hours following the exam.
To schedule peripheral artery disease treatment please speak with your doctor and call our interventional team at (512) 467-9729. A provider referral is required to make an appointment.
 Back to Top
Back to Top